Pleural Tapping

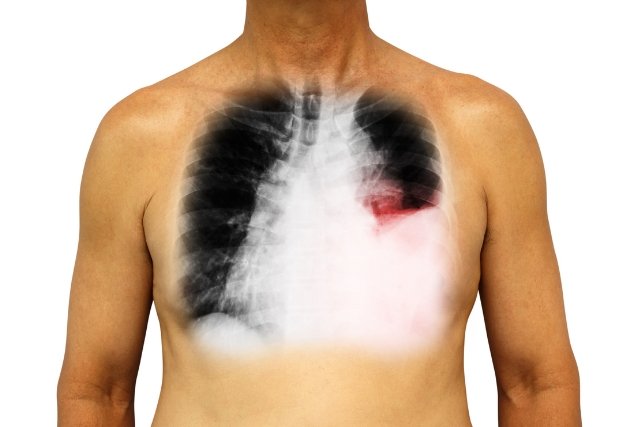
Ultrasound-guided pleural aspiration, also known as thoracentesis, is a diagnostic procedure used to remove fluid from the pleural space, the area between the lungs and the chest wall. This procedure is typically performed to aid in the diagnosis of various medical conditions affecting the lungs and pleura, such as pleural effusion (accumulation of fluid), pneumonia, cancer, or tuberculosis.
Here’s how the procedure typically works:
Preparation: The patient usually sits upright on the edge of a bed or examination table. The skin over the area where the needle will be inserted is cleaned and numbed with a local anesthetic.
Ultrasound Guidance: Before the needle is inserted, an ultrasound machine is used to locate the optimal site for aspiration. The ultrasound helps visualize the pleural space and any fluid accumulation, ensuring precise needle placement and reducing the risk of complications.
Insertion of Needle: Once the optimal site is identified, a thin needle attached to a syringe is inserted through the skin and into the pleural space. The needle is guided by real-time ultrasound imaging to ensure accurate placement and to avoid puncturing nearby structures such as blood vessels or the lung itself.
Fluid Collection: As the needle is inserted into the pleural space, fluid is withdrawn into the syringe. The amount of fluid collected depends on the underlying condition being investigated and may range from a few milliliters to several hundred milliliters.
Analysis: The collected fluid is sent to a laboratory for analysis. This may include testing for the presence of infection, cancer cells, blood, or other abnormalities.
Post-procedure Care: After the procedure, the needle is removed, and a bandage is applied to the insertion site. Patients are typically monitored for a short period to ensure there are no immediate complications, such as bleeding or pneumothorax (collapsed lung).
Ultrasound guidance has become a standard practice in pleural aspiration procedures as it improves safety and accuracy compared to traditional blind techniques. It allows healthcare providers to visualize the pleural space in real-time, increasing the success rate of the procedure and reducing the risk of complications.
